Leads ECG Placement: 7 Critical Mistakes to Avoid Now!
Understanding the correct leads ecg placement is crucial for accurate heart diagnostics. A small error can lead to misdiagnosis. Let’s dive into the essentials and avoid common pitfalls.
What Is Leads ECG Placement and Why It Matters

Leads ecg placement refers to the precise positioning of electrodes on the body to record the heart’s electrical activity. This process is fundamental in electrocardiography, a non-invasive test used globally to assess cardiac health. Incorrect placement can distort readings, leading to false interpretations of arrhythmias, ischemia, or myocardial infarction.
Anatomy Behind the ECG Signal
The heart generates electrical impulses that travel through specialized pathways. These impulses cause the myocardium to contract and pump blood. Electrodes placed on the skin detect these tiny voltages, which are then amplified and recorded by the ECG machine.
The standard 12-lead ECG uses 10 electrodes: 4 limb leads and 6 precordial (chest) leads. Each lead provides a unique ‘view’ of the heart’s electrical activity from different angles. For example, leads I, II, and III measure the heart’s activity in the frontal plane, while the precordial leads (V1–V6) capture horizontal plane activity.
“The accuracy of an ECG is only as good as the electrode placement.” – American Heart Association (AHA)
Impact of Incorrect Placement on Diagnosis
Misplaced electrodes can mimic or mask serious cardiac conditions. For instance, misplaced V1 and V2 electrodes can create patterns resembling right bundle branch block or anterior myocardial infarction. A study published in Circulation found that up to 40% of ECGs in emergency departments had at least one lead placement error.
- False ST-segment elevation or depression
- Misdiagnosis of myocardial infarction
- Inaccurate axis determination
- Incorrect identification of arrhythmias
These errors not only delay proper treatment but may also lead to unnecessary interventions, such as thrombolytic therapy or cardiac catheterization.
Standard 12-Lead ECG Configuration
The 12-lead ECG is the gold standard for cardiac assessment. Despite its name, it uses only 10 electrodes to generate 12 different electrical views (leads) of the heart. Understanding the configuration is essential for proper leads ecg placement.
Limb Leads: RA, LA, RL, LL
The four limb electrodes are placed on the arms and legs:
- RA (Right Arm): On the right upper limb, usually the wrist or upper arm.
- LA (Left Arm): On the left upper limb, symmetric to RA.
- RL (Right Leg): On the right lower limb, serves as the electrical ground.
- LL (Left Leg): On the left lower limb, completes the limb circuit.
These electrodes form the basis for the six limb leads: I, II, III, aVR, aVL, and aVF. Leads I, II, and III are bipolar, meaning they measure the voltage difference between two limbs. The augmented leads (aVR, aVL, aVF) are unipolar and use a combination of electrodes as a reference point.
Tip: Always place limb electrodes on the fleshy parts of limbs, avoiding bony prominences to reduce motion artifact.
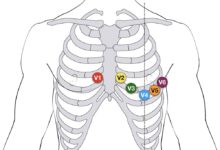
Precordial (Chest) Leads: V1 to V6
The six chest leads are placed in specific intercostal spaces across the chest wall:
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Horizontal to V4, anterior axillary line.
- V6: Horizontal to V4 and V5, midaxillary line.
These leads provide a horizontal view of the heart, crucial for detecting anterior, lateral, and septal infarctions. Misplacement of V4, for example, can shift the entire precordial progression, leading to misinterpretation of R-wave progression.
A common error is placing V4 too high or too lateral. The 5th intercostal space is just below the angle of Louis (sternal angle), which can be palpated at the 2nd rib. From there, count down two spaces to locate the correct position.
Common Errors in Leads ECG Placement
Despite standardized guidelines, errors in leads ecg placement are surprisingly common. A 2018 audit in a UK hospital found that 35% of ECGs had at least one misplaced electrode. These mistakes are often due to lack of training, time pressure, or patient anatomy challenges.
Misplacement of Precordial Leads
One of the most frequent errors is incorrect positioning of the precordial leads, especially V1 and V2. Placing them in the 3rd or 5th intercostal space can alter the ECG pattern significantly.
- V1 and V2 too high: Can mimic right ventricular hypertrophy.
- V1 and V2 too low: May mask right bundle branch block.
- V4 placed laterally: Distorts lateral lead readings (V5, V6).
A study in the Journal of Electrocardiology showed that even a 1-2 cm shift in V1 can change the QRS morphology enough to suggest arrhythmogenic right ventricular cardiomyopathy.
Reversal of Limb Electrodes
Limb lead reversals are another common issue. Right-left arm reversal is the most frequent and can dramatically alter the ECG:
- Lead I becomes inverted.
- Precordial leads may appear normal, but limb leads show abnormal patterns.
- Can mimic dextrocardia or incorrect axis deviation.
Always double-check the color coding: white (RA), black (LA), red (RL), green (LL). Using mnemonic devices like “Smoke Over Grass, Fire Red Come Down” (white over black, red over green) can help prevent errors.
leads ecg placement – Leads ecg placement menjadi aspek penting yang dibahas di sini.
Pro Tip: If lead I is predominantly negative, suspect limb lead reversal.
Special Considerations for Leads ECG Placement
While standard placement works for most patients, certain clinical scenarios require modifications. Understanding these variations is essential for accurate leads ecg placement in diverse populations.
ECG in Obese Patients
Obesity can make it difficult to locate anatomical landmarks. Excess adipose tissue may dampen electrical signals, leading to low-amplitude complexes.
- Use ultrasound guidance if needed to locate intercostal spaces.
- Ensure electrodes are placed on firm tissue, not over fat rolls.
- Consider using higher-gain settings on the ECG machine.
In morbidly obese patients, the diaphragm may be elevated, shifting the heart’s position. This may require adjusting V4 placement slightly higher than usual.
ECG in Women with Large Breasts
In women, large breasts can obscure the precordial landmarks. Placing electrodes underneath the breast can lead to signal attenuation and motion artifact.
- Lift the breast gently to place V3, V4, V5, and V6 on the chest wall.
- Use adhesive electrodes with strong hold.
- Document the placement technique in the patient’s record.
A 2020 study in Heart & Lung found that 60% of ECGs in women had misplaced chest leads due to improper breast displacement.
“Always prioritize anatomical accuracy over convenience.” – European Society of Cardiology (ESC)
Step-by-Step Guide to Correct Leads ECG Placement
To ensure accuracy, follow a systematic approach to leads ecg placement. This reduces variability and improves diagnostic reliability.
Preparation: Skin and Patient Positioning
Proper preparation is the first step to a high-quality ECG.
- Ask the patient to lie supine, arms at their sides.
- Clean the skin with alcohol wipes to remove oils and dead skin.
- Shave excessive hair if necessary to ensure electrode adhesion.
- Allow the skin to dry before applying electrodes.
Patient movement, talking, or shivering can introduce artifact. Ensure the room is warm and the patient is relaxed.
Execution: Placing the Electrodes
Follow this sequence for optimal results:
- Locate the 2nd intercostal space using the sternal angle.
- Place V1 and V2 at the 4th intercostal space on either side of the sternum.
- Place V4 at the 5th intercostal space, midclavicular line.
- Place V3 midway between V2 and V4.
- Place V5 and V6 horizontally aligned with V4.
- Attach limb electrodes on the wrists and ankles (or upper arms and lower legs if distal placement is uncomfortable).
- Connect the cables according to color coding.
Double-check each electrode’s position before starting the recording. Use anatomical landmarks, not measurements from previous ECGs.
Remember: Consistency across serial ECGs is key for monitoring changes over time.
Verification and Troubleshooting
After placing the electrodes, verify the setup before recording. This step can prevent repeat tests and ensure diagnostic accuracy.
Checking for Artifacts and Noise
Common artifacts include:
- 60 Hz interference (from electrical sources): Appears as fine, regular oscillations.
- Wandering baseline: Caused by poor electrode contact or breathing motion.
- EMG noise: From muscle tremors or shivering.
To reduce noise:
- Ensure all electrodes are securely attached.
- Keep limb leads away from muscle masses.
- Use a ground electrode (RL) properly.
If the baseline is unstable, recheck skin preparation and electrode placement.
Using Lead I and aVR to Detect Reversals
Lead I should normally be positive. If it’s negative, suspect right-left arm reversal. In this case:
- aVR becomes upright instead of inverted.
- Lead II and III switch places.
Similarly, left arm-right leg reversal can mimic inferior infarction. Always review the limb leads for consistency.
Quick Check: In a normal ECG, P waves should be upright in leads I, II, and aVF.
Advanced Techniques and Alternative Placements
In certain clinical situations, standard leads ecg placement may not suffice. Advanced techniques can provide additional diagnostic information.
leads ecg placement – Leads ecg placement menjadi aspek penting yang dibahas di sini.
Right-Sided ECG for Right Ventricular Involvement
In suspected right ventricular infarction (often with inferior MI), right-sided leads (V4R to V6R) are essential.
- V4R: 5th intercostal space, midclavicular line on the right side.
- V5R and V6R: Horizontal to V4R.
ST elevation in V4R is a sensitive marker for right ventricular infarction and guides fluid management.
Reference: American College of Cardiology guidelines recommend V4R in all patients with inferior STEMI.
Posterior Leads (V7–V9)
Posterior myocardial infarction may not show changes in standard leads. Posterior leads can detect these:
- V7: Posterior axillary line, same level as V6.
- V8: Tip of the scapula.
- V9: Paraspinal area.
Posterior MI often shows ST depression in V1–V3, which resolves when posterior leads are added.
“Don’t overlook the posterior wall—silent but deadly.” – Dr. Eric Prystowsky, Cardiac Electrophysiologist
What is the correct placement for lead V1 in leads ecg placement?
Lead V1 should be placed in the 4th intercostal space at the right sternal border. This position is critical for accurately recording electrical activity from the right ventricle and septum.
How can limb lead reversal affect an ECG reading?
Limb lead reversal, especially of the arms, can invert lead I and alter the appearance of other limb leads. This may mimic conditions like dextrocardia or incorrect axis deviation, leading to misdiagnosis.
Why is proper leads ecg placement important for diagnosing heart attacks?
Accurate leads ecg placement ensures that ST-segment changes, Q waves, and T-wave inversions are correctly identified. Misplacement can mask or mimic myocardial infarction patterns, delaying life-saving treatment.
Can ECG lead placement differ in women?
Yes, in women with large breasts, precordial leads V3 to V6 should be placed on the chest wall beneath the breast tissue, not on the breast itself, to ensure accurate signal detection.
What should I do if the ECG shows excessive noise or artifact?
Check electrode adhesion, ensure the skin is clean and dry, minimize patient movement, and verify proper grounding. Repeating the ECG with improved technique often resolves the issue.
Proper leads ecg placement is not just a technical step—it’s a cornerstone of accurate cardiac diagnosis. From understanding anatomical landmarks to avoiding common errors and adapting to special cases, every detail matters. By following standardized protocols and verifying each step, healthcare providers can ensure reliable ECG results that guide effective patient care. Whether you’re a student, nurse, or physician, mastering leads ecg placement is a skill that saves lives.
leads ecg placement – Leads ecg placement menjadi aspek penting yang dibahas di sini.
Further Reading: